Five-step guide to healthcare lighting compliance—identify codes, audit systems, design retrofits, install/test, and document maintenance.


Healthcare lighting retrofits are challenging because they must meet strict safety, energy efficiency, and clinical standards. From operating rooms requiring intense lighting for precision to patient areas needing soft, tunable light for comfort, every space has unique needs. This guide simplifies compliance into five steps:
Proper planning ensures safety, energy savings, and compliance without disrupting patient care. Partnering with experts can streamline the process and help address complex requirements.
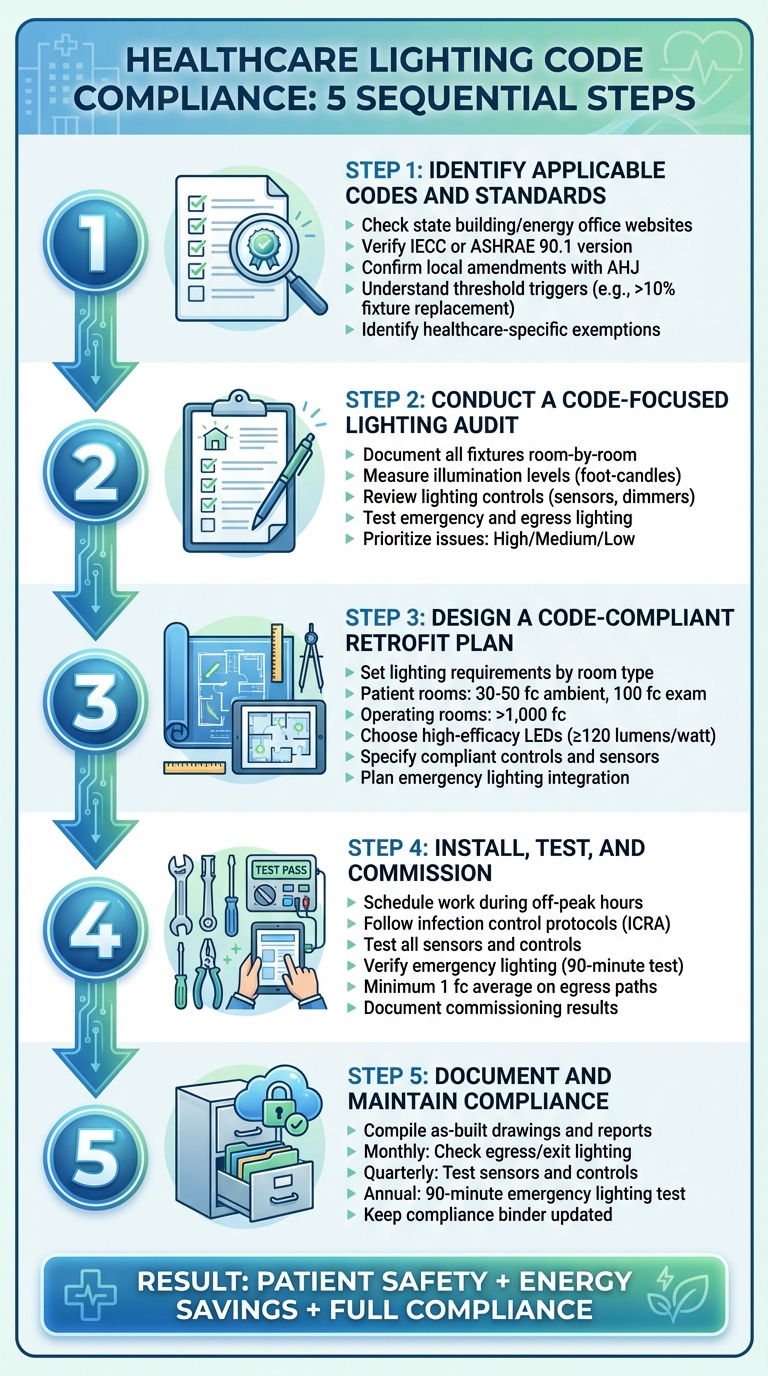
5 Steps for Healthcare Lighting Code Compliance
Before diving into a healthcare lighting project, it’s crucial to figure out which codes and standards apply. Healthcare facilities operate under a maze of regulations that differ by state, county, and even city. There’s no single “healthcare lighting code” to follow. Instead, you’ll need to juggle overlapping energy, safety, and clinical standards to ensure everything is compliant.
Start by checking your state building or energy office website for the version of the International Energy Conservation Code (IECC) or ASHRAE 90.1 that’s in effect. Then, confirm if there are any local amendments with your local authority having jurisdiction (AHJ). States update these codes on different schedules, so while a facility in Texas might be following IECC 2021, a hospital in California could be adhering to Title 24 2025. Make sure to verify the exact edition and its effective date.
Your local AHJ - usually the city or county building department - will be a key resource. Local amendments can significantly change state codes, especially when it comes to healthcare facilities. For example, ask them which NFPA 101 edition applies to emergency and egress lighting in your area and whether there are any specific exceptions for patient care spaces. Keep a record of these conversations, such as emails or screenshots, to create a clear paper trail. This will help your design team and make inspections smoother later on.
If you’re working on a facility in California, you’ll also need to consult the Healthcare Associated Infection Control and Abatement (HCAI) office. They publish specific timelines and exceptions for healthcare code adoption that might override some Title 24 requirements. Other states may have similar healthcare regulators within their departments of health.
This groundwork is essential for understanding when a full retrofit must meet compliance standards.
Not every lighting project triggers full compliance with current codes. For example, like-for-like maintenance, such as replacing a failed lamp or ballast with the same type and wattage, is typically considered routine and doesn’t require updates to meet current standards.
However, many energy codes use threshold triggers to determine when compliance becomes mandatory. These triggers vary, so check with your AHJ to understand the criteria. It might be based on the percentage of fixtures replaced, circuit load, or total wattage. For instance, in some jurisdictions, replacing more than 10% of fixtures in a single space could classify the project as a regulated alteration, requiring compliance with current lighting power density (LPD) limits and automatic controls for the entire area.
Additionally, confirm whether certain spaces qualify for healthcare-specific exemptions. Patient care areas often have exceptions from automatic shutoff or multi-level control requirements because continuous lighting is critical for safety. Lighting used for exams, surgeries, night lighting, or integrated into medical equipment may also be excluded from LPD calculations.
Knowing these thresholds will guide your retrofit planning and design decisions.
Once you’ve gathered all the relevant codes, create a reference table to keep everything organized for your team. Include columns for the code name and edition (e.g., "IECC 2021", "NFPA 101-2018"), jurisdictional details (state-adopted, local amendments, healthcare-specific exemptions), and the specific requirements that impact your project, such as LPD limits, required control types, egress lighting levels, and emergency backup durations.
Add another column for retrofit implications to summarize the compliance requirements tied to specific design decisions. For example: “If more than 40% of corridor fixtures are replaced, apply current LPD and automatic shutoff controls” or “Patient rooms exempt from multi-level controls but require manual on/off switches.” This table will serve as a quick reference during audits, fixture selection, and control zoning, ensuring no detail is overlooked.
Luminate Lighting Group offers a code landscape review during the scoping phase of a project. They can identify the governing energy code, verify local amendments with the AHJ, and build a compliance reference table before design begins. This upfront effort can save you from costly redesigns and help ensure your retrofit plan aligns with every applicable standard from the start.
Once you've identified the relevant codes, the next step is to perform a detailed audit. This audit will document your existing lighting systems, evaluate their performance against code requirements, and pinpoint areas that need improvement. The results will directly shape your retrofit design and help you prioritize updates.
Begin by creating a room-by-room inventory of fixtures. Walk through every space and note key details: fixture type (e.g., 2x4 recessed troffer, downlight, exam light), lamp technology (fluorescent, HID, LED), wattage, mounting height, and approximate age. Be thorough - include less obvious spaces like storage closets, mechanical rooms, and back corridors, as these areas contribute to the overall lighting power density (LPD) and may lack proper controls. Mark fixture locations on your floor plans to simplify LPD calculations later.
Next, measure illumination levels with a calibrated light meter (in foot-candles). For workspaces like desks or exam tables, take readings 30 inches above the floor. For egress paths, measure at floor level. Check multiple points - center, corners, and task areas - to assess both brightness and uniformity. Healthcare settings often require higher lighting levels than offices. For instance, patient rooms typically need 100 foot-candles at task areas, while surgical suites may exceed 1,000 foot-candles. Compare your readings to recommendations from ANSI/IES RP-29-22 and the IES Lighting Handbook for specific space types (e.g., patient rooms, operating rooms, imaging areas, pharmacies, corridors, and nurse stations). Document any areas where light levels fall short, as these could present safety risks even if they don’t explicitly violate codes.
Pay special attention to emergency and egress lighting. Identify which fixtures are connected to life safety or emergency circuits and verify that stairwells, egress paths, and exit discharge areas meet NFPA 101 requirements for illumination. Check that exit signs are visible, illuminated, and backed up by reliable power sources (battery, inverter, or generator) with the required run times. Address any emergency lighting deficiencies immediately, as these are critical for safety.
Once you've documented the performance of the existing system, turn your attention to verifying how the controls are functioning.
Take inventory of all control systems and their locations, including manual switches, occupancy or vacancy sensors (wall- or ceiling-mounted, dual-technology), time scheduling systems, daylight sensors, local dimming controls, and centralized or networked controls. For each space, confirm that the control strategy complies with applicable energy codes. For example, daylit zones with 75 watts or more of general lighting typically require automatic daylighting controls. Under Title 24 (2025), spaces larger than 100 square feet with general lighting exceeding 0.5 watts per square foot must support continuous dimming from 100% to 10% of full power, though healthcare facilities and specific light sources may have exceptions.
Test each control type to ensure it works as intended. For occupancy and vacancy sensors, walk through the space to verify coverage, time-delay settings (usually capped at 20 minutes by energy codes), and proper operation mode. For daylight-responsive controls, measure light levels with and without natural light to confirm that fixtures dim or switch off appropriately without causing glare or fluctuations. Document any faulty controls or settings that don’t align with energy code requirements, even if the hardware is installed.
Organize your audit findings into three categories: high, medium, and low priority.
To keep everything organized, create a compliance matrix that links each audited space to its applicable code requirements and current status (Compliant, Deficient, or Not Applicable). Use a standardized form or spreadsheet to track details like room ID, usage, fixture types and counts, measured light levels, control systems, and compliance notes. If you're in a Title 24 jurisdiction, plan ahead for Lighting Controls Acceptance Testing to ensure all control components installed during the retrofit will pass inspection. This matrix will be a crucial tool for guiding the design and installation phases that follow.
Luminate Lighting Group offers free on-site lighting assessments and energy audits for commercial, industrial, and public sector spaces. Their team documents existing fixtures, estimates potential energy savings, and models custom LED retrofit solutions - helping you identify your current energy usage and prioritize which compliance issues to address first.
Using the insights from your audit and compliance matrix, the next step is to create a retrofit design that meets both energy code standards and clinical lighting needs. This stage transforms the audit findings into actionable specifications, ensuring a balance between energy efficiency and practical lighting requirements for healthcare environments.
Define specific lighting performance targets for each room type, guided by standards like IES RP-29 and the FGI Guidelines for Design and Construction of Hospitals. For instance:
Document targets for illuminance, uniformity, color temperature (typically 3,000–4,000K for patient areas and 4,000–5,000K for clinical/task zones), and Color Rendering Index (CRI) to guide your design.
Select LED fixtures and lighting controls that align with both energy codes and clinical needs. U.S. energy codes, such as IECC and ASHRAE 90.1, set specific limits on lighting power density by space type. To meet these limits while achieving the necessary light levels, prioritize high-efficacy luminaires (120 lumens per watt or higher) with efficient light distribution.
A layered lighting approach - separating ambient, task, and exam lighting - can help achieve higher intensities only where they’re required, reducing overall energy consumption. For critical spaces like operating rooms, choose fixtures with sealed, cleanable housings, smooth lenses, and appropriate IP ratings to support disinfection protocols. In areas like exam rooms and patient rooms, low-glare optics improve visual comfort. Opt for DLC-listed or ENERGY STAR-certified products to potentially qualify for utility rebates.
Lighting control systems should comply with energy codes while supporting clinical workflows. Updated IECC guidelines require features such as occupancy or vacancy sensors, multi-level or continuous dimming, and daylight-responsive controls, especially in areas with connected loads over 75 watts. In 24/7 spaces like operating rooms and ICUs, pre-programmed lighting scenes with manual overrides ensure both safety and flexibility. Patient rooms should have separate controls for ambient, reading, and exam lighting, while administrative zones can adopt more aggressive energy-saving measures.
In some cases, manual switches and dimmers may need to be locked to prevent tampering. Collaborate with clinical staff during the design phase to ensure control strategies, such as automatic shutoff delays and dimming rates, align with patient care needs.
Once fixtures and controls are chosen, the focus shifts to incorporating emergency and life safety lighting.
Emergency lighting is a critical component of your retrofit plan. Ensure compliance with NFPA 101 by integrating emergency circuits, exit signage, and backup power systems. Identify all egress paths, stairwells, and critical care zones requiring emergency illumination. Depending on the facility's infrastructure and retrofit scope, decide whether to use centrally generator-supplied circuits for life safety branches or individual battery-backup fixtures. Address any deficiencies promptly, as this aspect of lighting design will be closely scrutinized during inspections.
Luminate Lighting Group specializes in creating custom lighting designs tailored to healthcare facilities. Their services include photometric layouts, fixture and control specifications, and compliance documentation, helping you meet IES, FGI, IECC, ASHRAE, and NFPA standards while optimizing clinical workflows and potentially qualifying for utility rebates.
Once the design is finalized, the next step is implementing the retrofit without disrupting day-to-day operations. This phase requires careful planning and execution to ensure patient care isn't interrupted. By following the approved design and audit findings, the installation process can be carried out efficiently, with a focus on maintaining safety and compliance.
Retrofitting systems in healthcare settings comes with unique challenges, especially when it comes to infection control. Before starting, it's essential to coordinate with infection prevention teams and facilities staff. This includes scheduling work during off-peak hours, nights, or weekends, setting up barriers, and establishing cleaning protocols to reduce risks in sensitive areas like operating rooms, ICUs, imaging suites, and pharmacies.
When work involves opening ceilings or drilling in patient zones, strict infection control measures are non-negotiable. Contractors must use barriers, HEPA-filtered negative air systems, and thorough cleaning to meet infection control risk assessment (ICRA) standards. Work zones should be clearly marked with signage and restricted access points, while tools, ladders, and cables must remain within the designated area to prevent hazards in hallways.
To maintain a calm environment, use low-noise, cordless tools, and schedule louder tasks outside of quiet hours. In critical areas like operating rooms, work is often performed between procedures, followed by terminal cleaning to ensure no compromise of fire or smoke barriers or medical gas systems. A phased approach - completing one zone at a time, testing it, and restoring full service before moving on - helps minimize disruptions and ensures proper lighting along egress paths.
"Our licensed electricians ensure full code compliance and minimal disruption to your operations." – Luminate Lighting Group
After installation, the focus shifts to testing and commissioning the system to validate its performance.
Once the system is installed, it's time to verify that everything operates as intended. Sensor placement, time-out intervals, and dimming stages must meet code requirements. Walk through the facility to confirm motion detection, ensure lights turn off after the programmed time-out (usually 15–30 minutes), and check partial-on or partial-off steps where applicable.
In healthcare settings, certain areas like patient rooms, imaging rooms, and operating rooms often have modified requirements for safety. The commissioning process should confirm that these spaces are controlled in a way that complies with codes while avoiding unsafe automatic darkening. Time delays should be long enough to prevent nuisance shutoffs in exam or procedure rooms but short enough to meet energy goals. Additionally, sensors managing egress paths or nurse workstations must ensure minimum lighting levels are maintained or restored promptly when occupancy is detected.
For daylight harvesting, photosensors need to be positioned away from direct sunlight and calibrated using a light meter. Adjust setpoints so that electric lighting dims smoothly as daylight increases, avoiding flicker or instability. Many energy codes require multi-level or continuous dimming, but in healthcare, these levels must align with clinical needs - such as exam, procedure, or nightlight modes in patient rooms. Scene presets should be simple for clinicians to use, with manual override switches conveniently located at nurse stations or room entrances. Under California Title 24 2025, hospitals may lock manual dimmers and switches in non-residential spaces to prevent unauthorized adjustments, while still allowing necessary overrides.
Both lighting controls and emergency systems need thorough post-installation verification to ensure full functionality.
Emergency lighting systems must meet the requirements of NFPA 101 Life Safety Code, NFPA 70 (NEC) Article 700, and CMS adoption of the 2012 Life Safety Code. Functional tests should simulate normal power loss, verifying that egress paths, stairwells, and exit signs illuminate properly. These systems must provide at least 1 foot-candle average and 0.1 foot-candle minimum along egress paths for at least 90 minutes.
Backup power systems - whether generators, inverters, or battery packs - should be tested in collaboration with the facility's electrical and clinical leadership. Generator transfer or battery-discharge tests should be scheduled during low-risk times. Healthcare providers are required to maintain detailed records of monthly quick tests and annual 90-minute tests, documenting dates, results, and any corrective actions to comply with NFPA 101 and CMS requirements. Any failures must be corrected and retested, with records kept ready for inspections by authorities or CMS surveyors.
Keep a comprehensive commissioning binder or digital record that includes as-built drawings, cut sheets, control schedules, test reports, and code references. This documentation is vital for inspections, accreditation visits, and utility rebate verification. Luminate Lighting Group handles every aspect of the retrofit process - from design and installation to testing and permitting - ensuring systems are optimized for long-term performance, energy efficiency, and code compliance.
Once installation is complete, keeping thorough records and adhering to established procedures is key to meeting energy codes, NFPA, and CMS standards. Compliance for healthcare lighting is an ongoing process. Facilities need to maintain documentation for inspections and perform regular testing to ensure they meet all necessary codes. Proper documentation and consistent maintenance help safeguard the integrity of your lighting retrofit, building on the groundwork laid during the audit and design phases.
After installation and testing, it's crucial to document every detail to ensure long-term compliance. Compile a comprehensive compliance package that includes all necessary documents. This package should feature:
Organize this information into a digital and hard-copy Lighting Compliance Binder, indexed by discipline - such as architecture, electrical, controls, and life safety. This makes it easy for inspectors and surveyors to find what they need during audits or accreditation visits. Store the digital version in a secure repository with controlled access and regular backups. Keep printed life-safety and egress plans accessible, ideally near the fire command center or as specified by your local authority.
Routine maintenance is essential to keep lighting systems functioning as intended and to prevent minor issues from escalating into compliance violations. Here's how to stay on top of maintenance:
Additionally, perform periodic illumination checks in critical areas like operating rooms, pharmacies, and nurse stations to verify that light levels remain within recommended ranges as fixtures age or room usage evolves.
Keep detailed records of all maintenance activities, including dates, responsible personnel, findings, and any corrective actions taken. Incomplete or missing test records can result in citations and mandatory corrective measures during inspections.
Develop a standard operating procedure (SOP) for any changes to the lighting system. This should clearly define roles and responsibilities, require a review of code implications before replacing fixtures or altering control zones, and establish approval thresholds for modifications affecting emergency lighting, patient-care areas, or control coverage. Update as-built drawings, control maps, and compliance logs after significant changes, using version control and date-stamping to ensure documentation reflects current conditions.
To help maintain compliance over time, professional assistance can make a big difference. Luminate Lighting Group offers services that go beyond installation, providing periodic reviews and updates to keep your lighting system aligned with changing codes. Their support includes post-occupancy evaluations of lighting performance, re-commissioning key areas, and updating sequences of operation to reflect changes in clinical workflows or regulations.
Luminate also helps with documentation management, such as updating lighting layouts, control hierarchies, and compliance records after renovations. They can guide you in structuring projects to take advantage of utility rebates and 179D tax deductions, all while ensuring healthcare lighting and life-safety standards are upheld. Their ongoing reviews and planning services help facilities stay ahead of code changes while maintaining safe, efficient, and compliant lighting systems for years to come.
To ensure compliance with healthcare lighting codes, follow these five key steps: identify the applicable codes (such as NFPA 101, NFPA 99, IES/ANSI RP-29-22, and state-adopted IECC or ASHRAE 90.1), conduct a detailed audit of your current lighting systems, develop a retrofit plan tailored to meet specific illuminance and control standards by room type, install and commission the new system with thorough testing of controls and emergency lighting, and document all testing while maintaining comprehensive records. This step-by-step process aligns with earlier guidance on audits, design, and installation, ensuring patient safety, regulatory compliance, and measurable energy savings.
Failing to meet NFPA 101 emergency lighting requirements or maintaining inadequate lighting can lead to clinical errors, patient falls, and accreditation issues. Noncompliance not only increases liability but can also jeopardize reimbursement. Outdated systems further compound the problem by wasting energy and driving up maintenance costs, making a strong case for modern LED-based, code-compliant upgrades.
Modern retrofit solutions address these risks while improving overall performance. While codes set the baseline, thoughtful retrofits elevate care environments. Advanced LED fixtures and cutting-edge controls enable features like task/ambient layering, scene customization, and tunable white lighting, which support both surgical precision and patient comfort - all while meeting strict energy standards.
For a seamless, code-compliant solution, consider partnering with Luminate Lighting Group. Their expertise spans every stage - from code-aware audits and custom healthcare lighting designs to licensed installation and emergency lighting integration. They also provide ongoing services to help facilities maintain documentation, update controls, and stay ahead of code changes, ensuring compliance over the system’s lifespan.
Start by conducting a focused audit to evaluate current conditions, identify compliance gaps, and estimate energy savings. Assemble a team that includes facilities management, clinical leaders, and safety compliance experts, and collaborate with a partner who understands NFPA life-safety requirements as well as state and local amendments. This initial step provides a clear budget, payback analysis, and a compliance risk overview, making it easier to secure capital planning and board approval while turning a complex challenge into an actionable plan.
Compliance in healthcare lighting involves meeting several critical codes and standards designed to ensure safety, efficiency, and accessibility. Key among these are the Illuminating Engineering Society (IES) guidelines, such as IES RP-29, which provides specific recommendations for lighting in healthcare settings. Similarly, the National Fire Protection Association (NFPA) codes, like NFPA 70 (National Electrical Code), focus on maintaining electrical safety in these environments.
In addition to these, adherence to the Americans with Disabilities Act (ADA) is crucial to guarantee accessibility for all individuals. Local building codes may also apply, depending on the region. Together, these standards work to ensure that healthcare lighting systems are not only functional but also safe and inclusive for everyone.
To keep disruptions to a minimum during a healthcare lighting retrofit, plan the work during off-peak times or scheduled maintenance windows. Opt for quick-install LED solutions to make the process faster and limit downtime. It's also crucial to collaborate closely with staff to ensure the project aligns with the facility's day-to-day operations and patient care priorities.
Working with experienced professionals who offer detailed planning and expert installation services can make the entire process smoother, helping to maintain regular operations with minimal interruptions.
Healthcare facilities often update their lighting systems for various reasons. These updates can stem from revised building codes, stricter energy efficiency standards, or newly introduced safety regulations. Advances in technology, like the development of LED lighting and modern control systems, also play a big role in pushing for upgrades to boost performance and ensure compliance. On top of that, regular facility audits or planned renovations often reveal chances to meet updated standards while enhancing the overall quality of lighting.